
Kudos has partnered with CardRatings and Red Ventures for our coverage of credit card products. Kudos, CardRatings, and Red Ventures may receive a commission from card issuers. Kudos may receive commission from card issuers. Some of the card offers that appear on Kudos are from advertisers and may impact how and where card products appear on the site. Kudos tries to include as many card companies and offers as we are aware of, including offers from issuers that don't pay us, but we may not cover all card companies or all available card offers. You don't have to use our links, but we're grateful when you do!
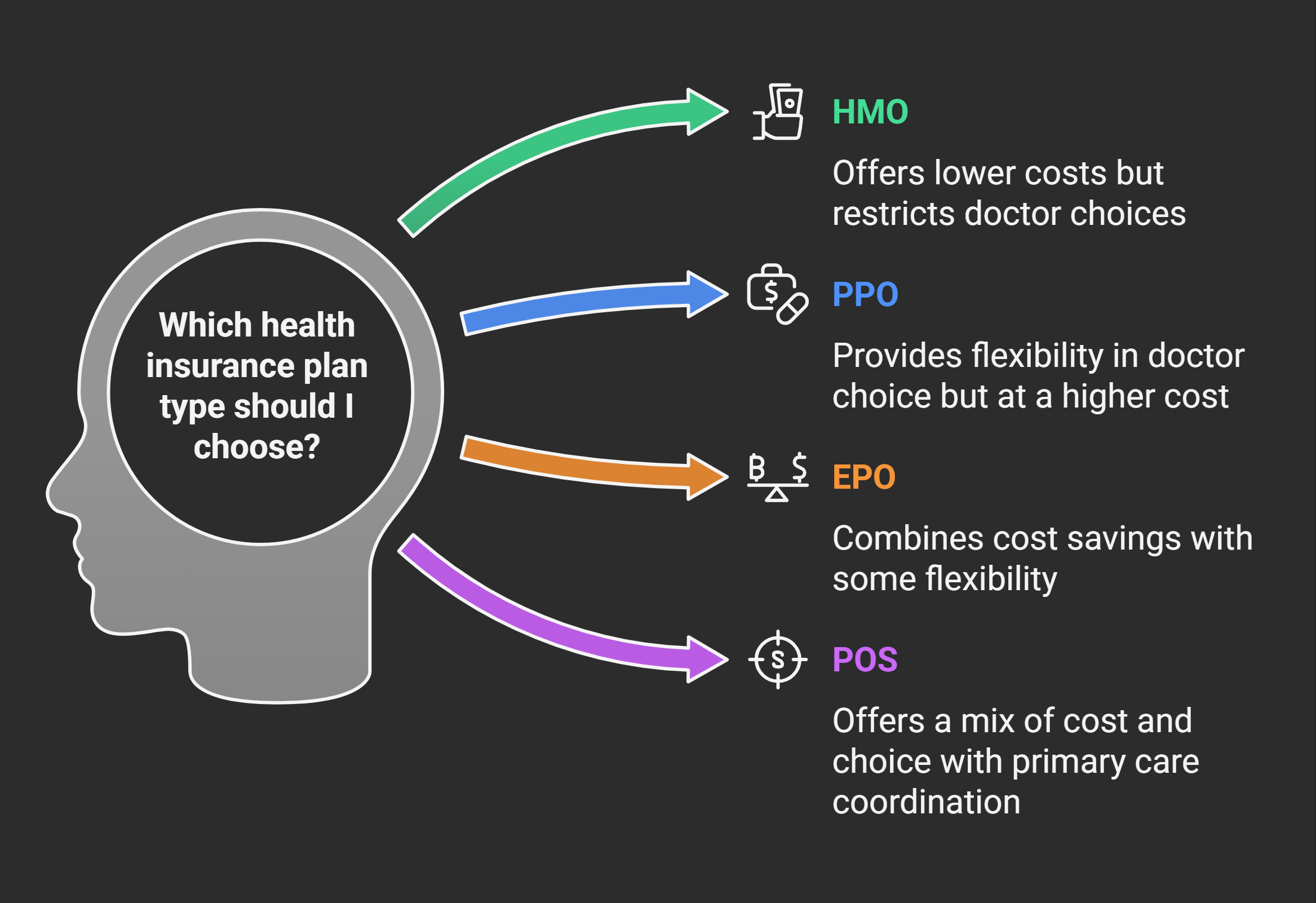
HMO vs PPO vs EPO vs POS: Choosing the Right Health Insurance Plan
July 1, 2025


When it comes to health insurance plans, an alphabet soup of acronyms can leave anyone confused. HMO, PPO, EPO, POS – what do these letters mean, and how do you decide which plan type is right for you? If you’re gearing up to choose a health insurance plan (for example, during open enrollment or at a new job), understanding the differences is key.
Some plans let you see any doctor but cost more, while others save you money but restrict your choices. In this comprehensive guide, we’ll break down the four common types of health insurance plans in the U.S. – HMO, PPO, EPO, and POS – explaining how each one works and the pros and cons.
By the end, you’ll be equipped to pick a plan that fits your healthcare needs and budget. No more mystery initials – let’s decode your health plan options!
Understanding the Basics of Plan Types
Before diving into each type, here’s a quick overview of what these acronyms stand for:
- HMO – Health Maintenance Organization
- PPO – Preferred Provider Organization
- EPO – Exclusive Provider Organization
- POS – Point of Service plan
All of these are types of managed care plans, meaning they contract with networks of doctors and hospitals. The core differences lie in how you access care and how flexible (or restrictive) the plan is about seeing providers outside the network.
Generally:
- An HMO is the most restrictive in provider choice and requires referrals to see specialists, but tends to have lower premiums and out-of-pocket costs.
- A PPO is more flexible – you can see specialists without referrals and go out-of-network (at a higher cost) – but premiums and costs are typically higher.
- An EPO is somewhat a hybrid: like an HMO it won’t pay for out-of-network care (except emergencies), but like a PPO you usually don’t need referrals for specialists. Premiums are in between.
- A POS plan is like an HMO with an escape hatch: you have a primary care doctor and need referrals, but you can go out-of-network if you’re willing to pay more (Point-of-Service). Costs are also in between.
Understanding these basics will help as we explore each plan type in detail. Now, let’s break down how each one works and for whom it might be a good fit.
HMO (Health Maintenance Organization)
An HMO is a plan that typically restricts you to a specific network of doctors and hospitals. With an HMO, you choose a Primary Care Physician (PCP) – usually a family doctor or internist – who coordinates all your care. If you need to see a specialist (like a dermatologist or orthopedist), you’ll first visit your PCP for a referral. HMOs generally do not cover out-of-network care except in emergencies.
If you go to a doctor or clinic outside the HMO’s network, you’ll likely have to pay the full cost yourself.
Advantages of HMOs:
- Lower costs: HMOs often have lower monthly premiums and out-of-pocket costs (copays, deductibles) than other plan types. They negotiate rates with a select network and manage care closely, which keeps costs down. If budget is your top concern, an HMO can be very attractive.
- Coordinated care: Having a primary doctor guide your care can be beneficial, especially if you like the idea of one point person managing your overall health picture. There’s less duplication of tests and better communication among your healthcare providers.
- Simplicity: Many HMOs have straightforward copays for most services and no complicated billing for out-of-network care (since you generally can’t use it). As long as you stay in-network, paperwork tends to be minimal.
Disadvantages of HMOs:
- Limited choice: The biggest downside is the lack of flexibility. You must use in-network providers. If you have a favorite doctor who isn’t in the HMO network, you’ll need to switch doctors or switch plans. For travelers or students, HMOs can be tricky because out-of-area coverage is usually only for true emergencies.
- Referral requirement: The extra step of seeing your PCP to get a referral to a specialist can be time-consuming. Some people don’t like needing “permission” to see a specialist. If you frequently need specialist care, this gatekeeping can be inconvenient (though some HMOs now allow direct specialist visits for certain services like OB/Gyn).
- Geographical focus: HMOs often operate in defined regions. If you split time between two states, for instance, an HMO might only cover one area.
Who might choose an HMO? If you’re looking for lower premiums and can work with a somewhat limited network of doctors – and you don’t mind the referral system – an HMO is a great choice. It’s often favored by individuals and families who have relatively predictable healthcare needs and whose doctors are already in the network. Many employer plans default to HMOs for cost savings. Just ensure you’re comfortable with the network and that key hospitals/clinics you’d use are included.
Remember, all plan types will cover you for essential health benefits (doctor visits, hospital, prescriptions, etc.) – the difference is how you access care and pay for it. There isn’t a universally “best” plan; it truly depends on your personal priorities.
PPO (Preferred Provider Organization)
A PPO plan offers much more flexibility in choosing providers. PPOs have a broad network of preferred providers (hospitals, doctors, specialists), but you are not required to stay in-network – it’s “preferred” but not mandated.
You also do not need a referral to see specialists; you can directly schedule appointments with any doctor you want. If you see an out-of-network provider, a PPO still covers part of the cost, although you’ll pay a higher share than if you stayed in-network.
Advantages of PPOs:
- Greater provider choice: You have wide freedom to pick doctors or facilities. If there’s a specific specialist you want to see who isn’t in your network, you can still go – the insurance will pay something (often around 50-70% after deductible) for out-of-network services. This is valuable if you want access to a larger pool of providers or frequently travel and may need care in different cities.
- No referral hassle: You can make appointments with specialists directly. This can save time and is convenient if you’re knowledgeable about what specialist you need or are managing a condition that occasionally requires expert care. It puts more control in your hands.
- Broad network: PPO networks are often expansive already, so even within “preferred” providers you might have a lot of choices. Many PPOs include most hospitals in a region and a long list of doctors. The out-of-network option is a safety net if you venture outside that list.
Disadvantages of PPOs:
- Higher cost: Generally, PPOs have higher premiums than equivalent HMOs. You’re paying for that flexibility. You might also see higher deductibles or coinsurance. For example, a PPO might require you to pay 20% of costs in-network (after deductible) and 40% out-of-network, whereas an HMO might just have a flat copay. If you stick in-network, the costs can be similar to an HMO, but the premium difference is notable.
- More paperwork (possibly): If you do go out-of-network, sometimes you might have to file claims yourself to get reimbursed, since out-of-network providers might not bill your insurance directly. In-network, this usually isn’t an issue.
- Analysis paralysis: With freedom comes the need to make more decisions. Some people find it overwhelming to have so many choices. If you’re not sure how to find a good doctor, an HMO’s smaller network might be simpler, whereas a PPO leaves it wide open.
Who might choose a PPO? If you want flexibility and don’t mind paying a bit more for it, a PPO is ideal. It’s great for people who have specific doctors they insist on using (and those docs might not all be in one network), or for those who travel frequently or have children away at college – the nationwide coverage can be a relief.
It’s also a good choice if you anticipate needing specialists and prefer not to funnel all care through a primary doctor. In short, a PPO is about choice and convenience, and you pay for that in premiums. Many families opt for PPOs to ensure everyone can use the doctors they prefer.
EPO (Exclusive Provider Organization)
An EPO plan is somewhat of a middle ground between HMO and PPO. Like an HMO, an EPO generally does not cover out-of-network care (except emergencies). “Exclusive Provider” means you must use the providers in the EPO network. However, EPOs typically do not require referrals to see specialists. You can usually schedule specialist visits directly, as long as that specialist is in the network.
Advantages of EPOs:
- No referral needed: The big plus over an HMO is that you don’t need a primary care referral to see a specialist. This makes using your insurance more straightforward when you have specific health issues – you can go straight to, say, a cardiologist or allergist in the network.
- Medium cost: Premiums for EPOs tend to fall in between HMO and PPO costs. You’re saving compared to a PPO because you give up out-of-network coverage, but it might cost slightly more than an HMO in exchange for the increased flexibility of self-referral. It can be a nice balance of cost and freedom.
- Simplicity of network: Similar to an HMO, you have a defined network which often can simplify choices. Many EPO networks are quite extensive, sometimes comparable to PPO networks. If the network meets your needs, you likely won’t feel the difference.
Disadvantages of EPOs:
- No out-of-network coverage: Just like an HMO, you are locked into the network with an EPO. If you go outside, you pay full price. This can be limiting if you need a very specialized treatment not available in-network. Always check that any specific doctors or hospitals you might want are in the EPO’s list.
- May need pre-authorization: Even though referrals aren’t needed, certain procedures or expensive tests might require prior authorization from the insurance company. This is true in many plan types, but just something to be aware of – freedom from referrals doesn’t mean total freedom to get any service paid without pre-approval steps.
- Less common type: EPOs are not offered by all insurers in all regions, so depending on where you live or your employer’s options, you might not see an EPO option. They’ve grown more common on ACA marketplaces recently, but availability varies.
Who might choose an EPO? If you’re looking for a Goldilocks option – more choice than an HMO, but cheaper than a PPO – an EPO can be a great fit. It works well if you don’t want to bother with referrals and you’re confident the network has the providers you’ll use.
People who are generally healthy but want the freedom to see specialists directly often like EPOs. Just remember, you are trusting that network to meet your needs; if you have any favorite doctor out-of-network, you’ll either need to switch to one in-network or choose a different plan type.
POS (Point of Service)
A POS plan is like a hybrid of HMO and PPO features. With a POS, you do need a primary care physician and referrals to specialists, similar to an HMO. However, like a PPO, a POS plan does offer some out-of-network coverage – but usually you’ll pay a lot more for out-of-network than in-network. Think of POS as “HMO with an option to go out-of-network if you really want to (for a higher cost).”
Advantages of POS:
- In-network costs are low: When you use the plan like an HMO (staying in-network and getting referrals), you often enjoy low copays and deductibles. POS plans’ in-network structure is very HMO-like and usually quite affordable.
- Out-of-network option: If there’s a doctor you really want to see who isn’t in your network, a POS plan at least gives you some coverage for that visit, whereas an HMO would give none. Typically, a POS might reimburse 50-60% of out-of-network costs after a higher deductible. It’s a nice safety valve if you occasionally need to go out-of-network.
- PCP coordination: Some people value having a primary doctor coordinate everything (maybe you like your PCP a lot and trust their guidance). The POS keeps that model, which can result in well-organized care, especially if you have multiple specialists – your PCP can help coordinate referrals and keep track of the big picture.
Disadvantages of POS:
- Referral requirement: Just like HMOs, you’ll need referrals to see in-network specialists. This can slow down care or be a hassle if you frequently need specialized services.
- Out-of-network is pricey: Yes, you can go out-of-network, but the costs can be high. POS plans often have a separate, higher deductible for out-of-network, and higher coinsurance (the percentage you pay). You might have to pay the doctor up front and submit a claim for partial reimbursement. So the out-of-network benefit, while nice to have, shouldn’t be viewed as free reign – it’s more like an emergency option.
- Moderate premium: Premiums for POS plans tend to be in the middle (often similar to or slightly higher than EPO premiums). If you don’t actually use the out-of-network feature, you might wonder if the extra premium cost is worth it compared to an HMO.
Who might choose a POS? A POS plan could be a good choice if you appreciate the guided care of a primary doctor and mostly stay in-network, but you want the peace of mind that you could go out-of-network if something unusual came up. It’s somewhat niche – many people either prefer the full HMO style or jump to PPO for freedom.
But POS can make sense if, say, you’re in an HMO now and happy, but you know there’s a particular specialist not in the HMO network that you might need next year – a POS plan would let you see them (with referral and higher cost) without completely paying on your own. It offers a bit of flexibility without moving all the way to a higher-cost PPO.
Comparing the Plans: Which One Should You Choose?
Now that we’ve described each plan type, how do you decide which is right for you? Here are a few considerations to guide your choice:
Budget vs. Choice:
If keeping your monthly premium low is the top priority and you don’t mind limited choice, an HMO is likely your best bet. If you absolutely need freedom to choose or your providers are scattered, a PPO might be worth the extra cost. EPO and POS are middle options balancing cost and choice. Consider how much more you’re willing to pay for the ability to use out-of-network doctors or to self-refer to specialists.
Your Doctors:
Make a list of your current doctors (primary care, specialists, etc.) and check which plan networks include them. If all your doctors are in the HMO network, then an HMO could work well. If one of your important doctors is out-of-network, decide if you’re willing to switch doctors or if not, then maybe lean toward a PPO or a POS that would cover at least some visits to that doctor. If you don’t have strong attachments to specific providers, you have more flexibility to go with an HMO or EPO and just use who’s in-network.
Referral Preference:
Some people are okay with referrals (maybe they like their PCP coordinating things), while others find it cumbersome. If you hate the idea of needing a referral for a dermatologist visit, eliminate HMOs and POS from your list – stick to PPO or EPO. If referrals don’t bother you, then all types are still on the table.
Healthcare Needs:
Think about how often you use medical services. If you have a chronic condition requiring regular specialist care, a PPO might save you time since you can go straight to specialists, and a POS/HMO could mean frequent doctor visits just for referrals. Also, heavy medical users might value the ability to go out-of-network for second opinions at top facilities (point for PPO/POS). If you rarely go to the doctor, you might prioritize just the cost and convenience – maybe an HMO or EPO with low premium and straightforward copays is fine.
Geography and Travel:
If you travel a lot or have family in multiple states, a PPO can give you nationwide network access and out-of-network coverage that could be crucial on the road. An HMO or EPO might leave you with coverage gaps when traveling (except emergencies). Students who go out-of-state, for instance, might need a PPO so they can get care away from home campus.
Need for Specialists:
For families, consider each member – if one child needs a specific specialist frequently, ensure the plan supports that easily (either the specialist is in-network, or you have a PPO for out-of-network). If someone needs mental health counseling, check networks for those providers too.
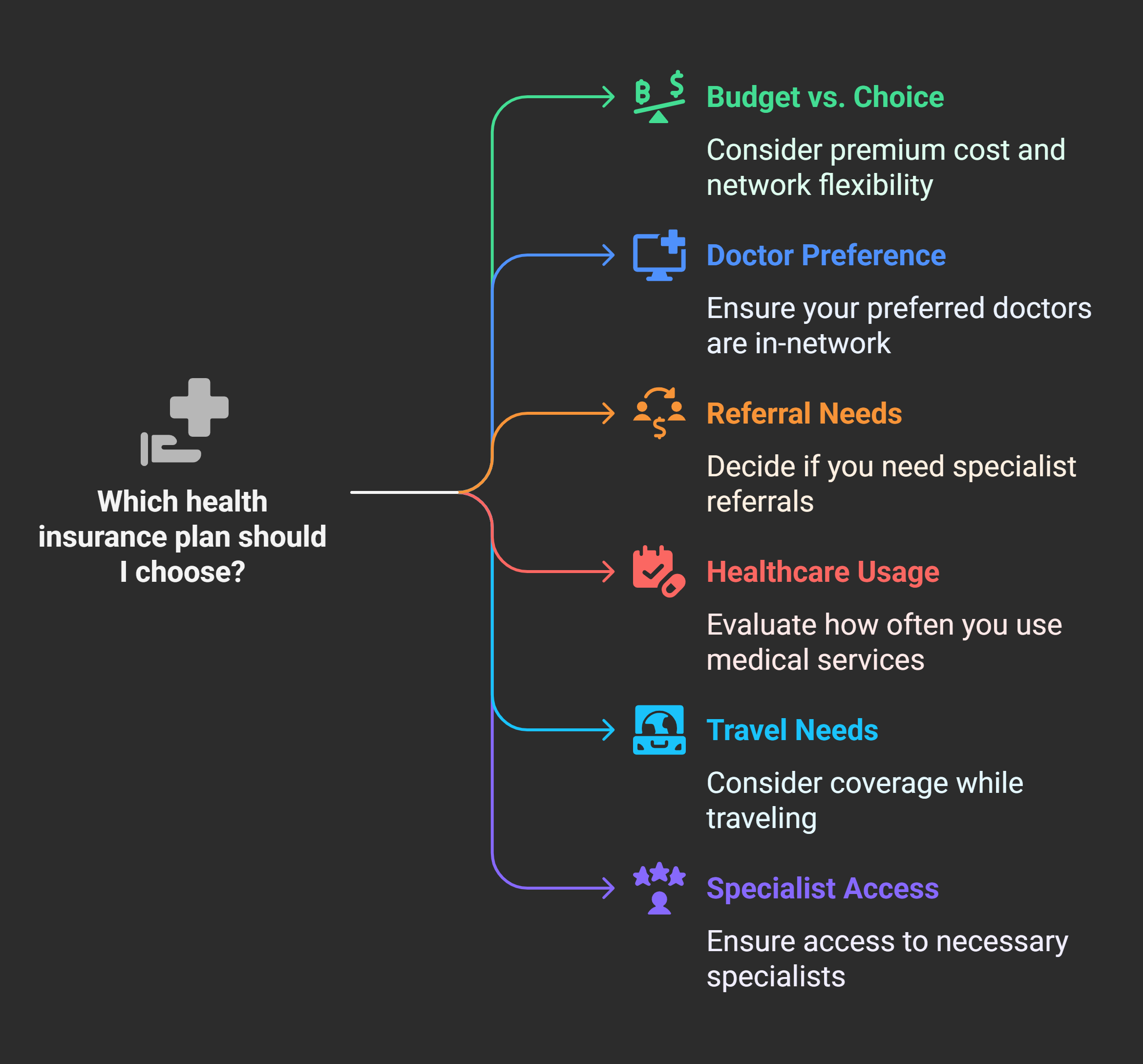
In many employer scenarios, the decision might come down to two options – e.g. “HMO vs PPO.” In that case, weigh how much more the PPO costs versus how much you value the flexibility. If it’s, say, $50 more per month, ask yourself if $600 a year is worth the ability to go out-of-network or skip referrals. For some, it is absolutely worth it; for others, $600 could be saved for other expenses.
Making the Most of Your Plan (Whichever Type It Is)
No matter which plan type you choose – HMO, PPO, EPO, or POS – a few tips can help you maximize your benefits and avoid extra costs:
- Stay in-network whenever possible: You will always save money by using in-network providers due to negotiated rates. Even on a PPO, try to use network doctors unless there’s a compelling reason not to.
- Build a relationship with your primary care doctor: This is crucial for HMO/POS plans (for referrals), but even in PPO/EPO, a good PCP can help coordinate care and give advice on specialists. They might also help you navigate insurance quirks.
- Understand your plan’s rules: If you have an HMO or POS, know the referral process. If you have a PPO or POS, know the out-of-network deductible and coinsurance so you aren’t shocked by a bill. If you have an EPO, remember not to go out-of-network except emergencies. Little rules (like needing pre-authorization for an MRI) are usually in the plan materials – taking a moment to skim those can save headaches later.
- Use tools to compare options: If you’re still unsure which plan to pick, consider using a comparison tool or advisor. Kudos, for example, can help you compare health plan options side by side. By inputting your doctors or medications, it can show which plan types cover them. It’s an easy (and free) way to visualize differences in cost and coverage before you commit to a plan.
- Reevaluate each year: As healthcare and your circumstances change, the ideal plan type for you might change. Maybe one year an HMO works great, but next year you develop a condition that requires more specialist care – you might switch to a PPO during the next enrollment. Don’t be afraid to change plan types if your needs shift.
By understanding the distinctions between HMO, PPO, EPO, and POS plans, you’ve already taken a big step toward making an informed insurance choice. The jargon may be intimidating, but at the end of the day, it boils down to a trade-off between cost and flexibility.
Consider what matters most to you, leverage the resources at your disposal (like Kudos or your HR’s guidance), and you’ll be able to choose a health insurance plan with confidence.
FAQs: HMO, PPO, EPO, POS
Which is better, an HMO or a PPO?
Neither is universally “better” – it depends on your needs. An HMO is better if low cost is your priority and you’re okay with using a set network of doctors and getting referrals for specialists. A PPO is better if you value flexibility – you can see any doctor, including out-of-network (some coverage provided), and you don’t need referrals. Think of HMO as a budget-friendly, managed approach, and PPO as a convenience and choice-oriented approach.
What is an EPO plan in simple terms?
An EPO (Exclusive Provider Organization) is like a blend of HMO and PPO. In simple terms: an EPO requires you to stay in-network (like an HMO – it generally won’t pay for out-of-network care), but does not require referrals to see specialists (like a PPO – you can directly visit any in-network specialist).
Do I need a referral with a POS plan?
Yes. A POS (Point of Service) plan generally functions like an HMO when you’re using it in-network, meaning you do need a referral from your primary care physician to see a specialist in-network. The “point of service” refers to the fact that when you actually go to get care (“at the point of service”), your costs depend on whether you stayed in-network (lower cost, with referral) or went out-of-network (higher cost). So for in-network services on a POS, you will see your primary doctor first to get a referral, similar to the HMO model.
Are premiums lower for HMOs than PPOs?
Typically, yes, HMO premiums tend to be lower than PPO premiums for a similar level of coverage. This isn’t a hard-and-fast rule, but generally because HMOs restrict providers and manage care tightly, they save costs and pass those savings in the form of lower premiums. PPOs, offering more flexibility, usually cost more.
If I have a rare medical condition, what plan type is advisable?
If you have a rare or complex medical condition, you may need access to a wide range of specialists and possibly out-of-state medical centers. In this case, a PPO plan is often advisable. The PPO’s flexibility means you can seek care from top specialists anywhere and still have some coverage.
Unlock your extra benefits when you become a Kudos member

Turn your online shopping into even more rewards

Join over 400,000 members simplifying their finances

Editorial Disclosure: Opinions expressed here are those of Kudos alone, not those of any bank, credit card issuer, hotel, airline, or other entity. This content has not been reviewed, approved or otherwise endorsed by any of the entities included within the post.






























.webp)







